Lysergic acid diethylamide (LSD), is a molecule whose history is as fascinating as its powerful effects on the brain. Acid Dreams, written by Martin A. Lee and Bruce Shlain is a wonderful resource for the former (history). Where as this blog post is designed to touch on the later (LSD's effects on the brain; primarily, LSD's role in hallucinations).
Serotonin in Disguise
One reason that LSD (a potent hallucinogen) causes hallucinations is because it mimics a neurotransmitter. A neurotransmitter is a molecule released from the ends of a neuron, neurons are the tiny cells which make up the nervous system. Once released, the neurotransmitters bind to specific receptors on an opposing neuron. The release of various neurotransmitters occurs all throughout the brain, and it is the means for communication between neurons. The neurotransmitter in which LSD mimics is serotonin (5-HT). As the photograph of Dr. Albert Hofmann is demonstrating, LSD and serotonin both share an important chemical bond[1].
Which Receptor?
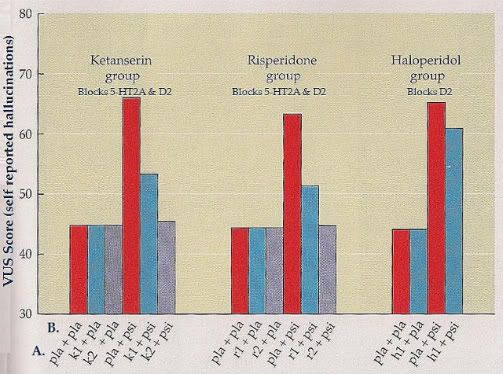
So LSD mimics serotonin, but how does that cause hallucinations? A widely accepted answer is that LSD binds to particular serotonin receptors, it does not bind to all of the serotonin receptor subtypes. In particular the 5-HT2A subtype has been at the forefront of investigation. A seminal study in the implication of the role of 5-HT2A was conducted by Vollenweider and colleagues (1998). These researchers exposed participants to various antipsychotics (medication used to treat schizophrenia) prior to the ingestion of a chemical similar to LSD - psilocybin. The antipsychotics that effectively reduced hallucinations worked by blocking the 5-HT2A receptors[2]. The antipsychotic that did not reduce hallucinations only blocked the dopamine receptors (D2 subtype). Therefore, suggesting the 5-HT2A receptor to be the likely source of hallucinations caused by hallucinogens (FIG. 1).
on the Y axis. Antipsychotic condition is represented by A. on the X axis; placebo antipsychotic (pla), ketanserin (k1 = 20
mg, k2 = 40 mg of ketanserin), risperidone (r1 = 0.5 mg, r2 = 1.0 mg), and haloperidol (h1 = 0.021 mg/kg). Hallucinogen
condition is represented by B. on the X axis (pla = placebo hallucinogen, psi = psilocybin). Figure and text adopted from: Meyer and Quenzer (2005).
Description of Above Figure
When participants received a placebo hallucinogen, participants reported mild VUS Scores. However, when the placebo antipsychotic was administered with psilocybin, VUS Scores were elevated. Both ketanserin and risperidone were effective at reducing VUS Scores. However, halperidol was not effective at reducing VUS Scores. The main pharmacological difference between these antipsychotics is the receptor in which they antagonize (block). Ketanserin and risperidone both block 5-HT2A as well as D2 receptors, while halperidol blocks only D2 receptors. Halperidoldid not reduce VUS Scores, therefore the decrease in VUS Scores from ketanserin and risperidone can be accounted for by the blockage of the 5-HT2A receptor.
In addition, when the 5-HT2A is blocked, researchers have found that rats will decrease the self administration of LSD [3]. This finding suggests the positive reinforcing mechanism lies within the activation of the serotonin receptor. This is an interesting finding as many other psychoactive drugs influence addiction by way of the dopamine system.
Which Brain Structures?
To gain a complete picture of LSD's role in hallucinations, it is also important to consider what brain location is influenced by LSD. Vollenweider and Geyer (2001) suggest the effects (including hallucinations) produced by LSD are caused by an improper filtering of sensory material reaching the cortex. In other words, the cortex which is the outer region of the brain, is receiving too much information. Neuroimaging techniques implicated various structures such as the frontal cortex, striatum, and thalamus [4]. These areas respectively are important in decision making, feelings of reward, and the routing of sensory information related to vision, hearing, and touch.
In a case study, researchers measured brain activity of an individual who experienced visual hallucinations without the presence of LSD [5]. This individual experienced the hallucination of a face when he viewed trees, the authors believe this abnormality likely arose after many years of illicit drug use. Using functional Magnetic Resonance Imaging (fMRI), researchers found an increase in activation of a visual processing area important in the perception of a face. This area is called the fusiform face area and activation of it allows for the recognition of faces. This activation can be seen in figure 2.
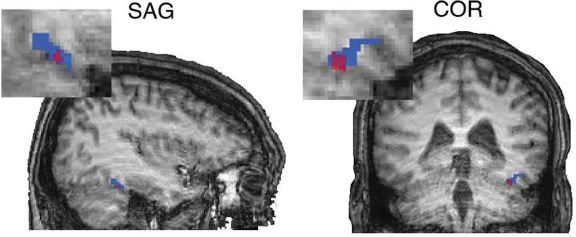
Figure 2. Activity of the fusiform face area is shown in a sagittal plane (SAG) and a coronal plane (COR). Hallucination of a face is demonstrated via blue, whereas activation of an actual face is demonstrated with magenta.
Conclusion
This brief review of LSD and hallucinations is only a small section of a much larger piece of literature. While 5-HT2A activation appears to be influential in causing hallucinations, the brain areas associated with such hallucinations are not as well studied. If the reader requires more information on this topic, I would direct your attention to two recent review articles by Vollenweider and Kometer (2010) as well as Lee and Roth (2012). Their complete references can be found bellow in the sixth and seventh reference respectively.
References
1. Green, A., R. (2008). Gaddum and LSD: the birth and growthof experimental and clinical
neuropharmacologyresearch on 5-HT in the UK. British Journal of Pharmacology, 154,
1583-1599. doi: 10.1038/bjp.2008.207
2. Vollenweider, F. X., Vollenweider-Scherpenhuyzen, M. I., Bäbler, A., Vogel, H. & Hell, D. (1998)
Psilocybin induces schizophrenia-like psychosis in humans via a serotonin-2 agonist action.
Neuroreport, 9, 3897-3902. doi:10.1097/00001756-199812010-00024
3. Apple, J. B., West, W. B., & Buggy, J. (2004). LSD, 5-HT (serotonin), and the evolution of a
behavioral assay. Neuroscience & Biobehavioral Reviews, 27, 693-701.
doi:10.1016/j.neubiorev.2003.11.012
4. Vollenweider, F. X., & Geyer, M. (2001). A systems model of altered consciousness: Integrating
natural and drug-induced psychoses. Brain Research Bulletin, 56, 495-507.
doi:10.1016/S0361-9230(01)00646-3
5. Iaria, G., Fox, C. J., Scheel, M., Stowe, R. M., & Barton, J. J. (2010). A case of persistent visual
hallucinations of faces following LSD abuse: a functional Magnetic Resonance Imaging study.
Neurocase: The Neural Basis of Cognition, 16, 106-118. doi:10.1080/13554790903329141
6. Vollenweider, F. X., & Kometer, M. (2010). The neurobiology of psychedelic drugs: implications for
the treatment of mood disorders. Nature Reviews Neuroscience, 11, 642-651.
doi:10.1038/nrn2884
7. Lee, H., & Roth, B. L., (2012). Hallucinogen actions on human brain revealed. PNAS, 109,
1820-1821. doi: 10.1073/pnas.1121358109